Learn how our private, nonprofit organization has become one of the largest women’s specialty hospitals in the United States and is recognized throughout the country for its innovative programs for women and their families.
A history of exceptional care, centered on you
1950s
- In the 1950s, the post war baby boom was in full swing, and a group of physicians saw a need for obstetric gynecologic care centered around the woman in Baton Rouge. Drs. Julius H. Mullins, Sr., Jack Jones and Cary Dougherty, along with 16 other physicians, dreamed of a facility that would be centered on the unique needs of women and newborn babies.
1960s
- In 1968, Woman’s opened its doors, becoming one of the first women’s specialty hospitals in the nation. We successfully performed three surgeries on our first day of operation.
1970s
- Woman’s was performing about two mammograms a day—usually for women who had a lump or other symptoms of breast cancer—when in 1973 a comprehensive study out of New York showed statistically significant improvements in breast cancer deaths for women who received mammograms.
1980s
- Woman’s opened its dedicated Breast Center in 1985 and performed 3,000 mammograms in the first year, emerging as an advocate for early detection and breast cancer awareness. Today, Woman’s performs more than 46,000 breast procedures each year.
1990s
- Radioactive tracers, which are injected to identify cancerous nodes, were the first in a series of technological advances in diagnostic breast imaging to be added in the late 1990s. This approach meant that women had the potential for a less invasive surgery and thus a lowered risk of lymphedema or swelling in one or both arms.
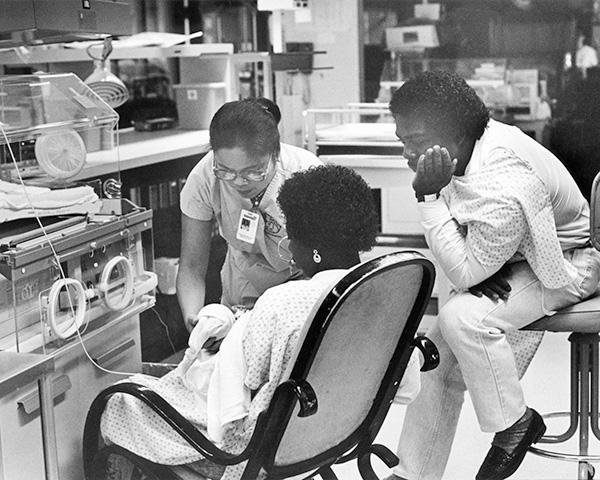
- In 1995, we established a helicopter transport service for high-risk mothers and critically ill infants. That same year, Woman’s NICU operating room opened, one of only a few in the country dedicated to infant surgery within a NICU. In 1998, the hospital joined the Vermont Oxford Network, the first large-scale initiative to develop a clinical database and create best practices that hospitals worldwide would use to improve the care of critically ill infants.
2000s
- In 2003, the Breast Center began using Computer-Aided Detection (CAD), which provided an additional review for detecting breast abnormalities. In 2005, mammography services were upgraded from film technology to digital.
- When the catastrophic Hurricane Katrina made landfall on the Louisiana coast in 2005, Woman’s coordinated the evacuation of premature and sick babies – many without their mothers because of the severity of their conditions – as well as pregnant and ill women from hospitals in New Orleans. Escorted by police, the neonatal transport team made several trips to the city by ambulance and helicopter to rescue infants, returning with stories of extreme heat, no electricity and limited supplies, medications, food and water. We brought families together who had been separated for days. We set up a shelter so families could rest, eat and receive clean clothes. Woman’s team ignored the clock and stayed if they were needed. In the weeks that followed, Woman’s clinical care team treated more than 1,100 patients and delivered more than 150 babies from the affected areas – more than double as many critically ill babies as usual. The hospital again served as the social coordinating organization to manage emergency evacuations during Hurricane Rita one month later, and during Hurricane Gustav in 2008.
2010s
- The most monumental shift in NICU care came in 2012 when Woman’s relocated new campus opened. The design reflects Woman’s core belief that neonatal intensive care should be centered on an infant’s individual needs; all rooms are single-family, which were designed to feel like a baby’s nursery so parents can bond with their baby just like they would at home. This setting allows parents to stay overnight with their baby in the days, weeks and even months ahead. It also decreases noise, reduces infection, and allows staff to tailor care to each baby’s needs. Eleven new rooms, including a room for twins, were added in 2017.
- Woman’s began performing fetal surgery in 2017. Fetal surgery specialists are uncommon in the region, with the closest medical specialists residing in Houston and Miami. Woman’s has the region’s only fetal surgery specialist, who is skilled in highly complex pregnancy surgeries while the baby is still in the womb. He and the fetal surgery team perform surgeries to correct conditions such as twin-to-twin transfusion syndrome, spina bifida and congenital pulmonary airway malformation.
- Woman’s expanded our Mammography Outreach Program in 2017 with the addition of a second coach with 3D mammography to better serve the region. This program began in the mid-1990s, when an alarming pattern of higher breast cancer rates in rural and underserved areas emerged. Thousands of women lived in parishes with no access to mammography, so Woman’s outfitted two vans with mammography equipment and drove them to local businesses, churches and community centers.
- In 2012, Woman’s relocated all services to its 100 Woman’s Way. Our campus is designed to provide the most innovative care in an environment that welcomes families. Our soothing, healing atmosphere is focused on meeting women’s and infants’ needs.
2020s
- Today, Woman’s ranks 17th in the country in total births, with more than 8,500 deliveries each year. Woman’s is recognized throughout the country for its innovative programs for women and their families.